Search results for: 'blog a guide to coronavirus funds available to hospitals and universities'
-
 Super TORY® Neonatal Care SLE Facilitator’s Guide11120156CLearn More
Super TORY® Neonatal Care SLE Facilitator’s Guide11120156CLearn MoreThe Super TORY® Neonatal Care Simulation Learning Experiences™ (SLEs) Facilitator’s Guide is a comprehensive resource for planning, setting up, and facilitating scenarios with Super TORY® S2220. The Facilitator’s Guide makes it easier to consistently create immersive newborn patient care environments and facilitate training sessions.
-
 Pediatric HAL® SLE Facilitator’s Guide11120146CLearn More
Pediatric HAL® SLE Facilitator’s Guide11120146CLearn MoreThe Pediatric HAL® Advanced Pediatric Patient Simulation Learning Experiences™ (SLEs) Facilitator's Guide is a comprehensive resource for planning, setting up, and facilitating scenarios with Pediatric HAL® S2225. The guide makes it easier to consistently create immersive patient care environments and facilitate pediatric care training sessions.
Compatible with Pediatric HAL® S2225. -
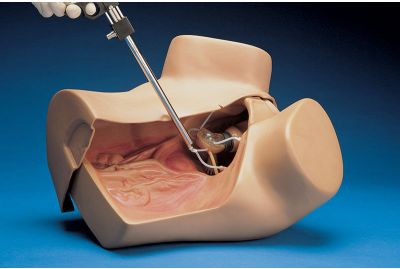
 Hysteroscopy Simulator (S607)S607.PKLearn MoreThe Hysteroscopy Simulator is an adult-sized female lower torso skills trainer used to practice proper hysteroscopy procedures. The S607 is designed with lifelike features that simulate the feel of the anterior pelvic wall and allow students to examine various internal and external pathologies. Participants can also use real equipment like a hysteroscope to work hands-on and improve their diagnostic and clinical skills.
Hysteroscopy Simulator (S607)S607.PKLearn MoreThe Hysteroscopy Simulator is an adult-sized female lower torso skills trainer used to practice proper hysteroscopy procedures. The S607 is designed with lifelike features that simulate the feel of the anterior pelvic wall and allow students to examine various internal and external pathologies. Participants can also use real equipment like a hysteroscope to work hands-on and improve their diagnostic and clinical skills. -
 Deep Vein Thrombosis Leg for VICTORIA® S2200S2200.101LLearn More
Deep Vein Thrombosis Leg for VICTORIA® S2200S2200.101LLearn MoreThe Deep1 Vein Thrombosis (DVT) package for VICTORIA® provides an additional complication to simulated labor and delivery scenarios and further expands the capabilities of the VICTORIA® advanced birthing simulator. Custom scenarios are available for diagnosing and treating DVT, and a library of drugs is available for simulated treatment options.
-
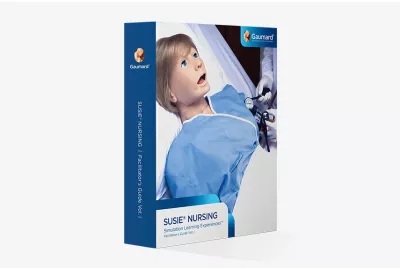
 SUSIE® Nursing SLE Facilitator’s Guide VOL. 211120151DLearn MoreThe SUSIE® Nursing Simulation Learning Experiences™ (SLEs) Facilitator’s Guide Vol. 2 is a comprehensive resource for planning, setting up, and facilitating advanced nursing scenarios with SUSIE®. The Facilitator’s Guide makes it easier to consistently create immersive patient care environments and facilitate training sessions.
SUSIE® Nursing SLE Facilitator’s Guide VOL. 211120151DLearn MoreThe SUSIE® Nursing Simulation Learning Experiences™ (SLEs) Facilitator’s Guide Vol. 2 is a comprehensive resource for planning, setting up, and facilitating advanced nursing scenarios with SUSIE®. The Facilitator’s Guide makes it easier to consistently create immersive patient care environments and facilitate training sessions.
Compatible with the following SUSIE® models: S2000. -
 SUSIE® Nursing SLE Facilitator’s Guide VOL. 111120150DLearn MoreThe SUSIE® Nursing Simulation Learning Experiences™ (SLEs) Facilitator’s Guide Vol. 1 is a comprehensive resource for planning, setting up, and facilitating scenarios with SUSIE®. The Facilitator’s Guide makes it easier to consistently create immersive patient care environments and facilitate training sessions.
SUSIE® Nursing SLE Facilitator’s Guide VOL. 111120150DLearn MoreThe SUSIE® Nursing Simulation Learning Experiences™ (SLEs) Facilitator’s Guide Vol. 1 is a comprehensive resource for planning, setting up, and facilitating scenarios with SUSIE®. The Facilitator’s Guide makes it easier to consistently create immersive patient care environments and facilitate training sessions.
Compatible with the following SUSIE® models: S1001 and S901. -
 SUSIE® Series (S901, S1001) - Male Chest Skin3001165Learn MoreThis accessory converts SUSIE® into a male patient, allowing for diverse simulated patient encounters. The chest skin supports four-lead ECG monitoring using real heart monitors.
SUSIE® Series (S901, S1001) - Male Chest Skin3001165Learn MoreThis accessory converts SUSIE® into a male patient, allowing for diverse simulated patient encounters. The chest skin supports four-lead ECG monitoring using real heart monitors.